By Tatjana van der Krabben
On May 30, 2015 I attended the 5th Dutch Lipedema Day in the lovely southern part of the Netherlands. It’s impossible to cover everything I heard and learned that day. In this blog I will point out some interesting facts and figures I picked up that day.
The first lecture was by dr. Veraart, dermatologist at the Academic Hospital of Maastricht, the Netherlands. At lightning speed he covered some interesting facts and figures:· Lipedema is very uncommon in South East Asia. At the same time most cases are reported in the western world.
This I’ve heard before. Estimates about the percentage or number of women affected worldwide vary and they vary for a reason. 11% of all women across the globe most likely is NOT accurate. Careful what you quote out there.· There is no hard classification to describe lipedema.
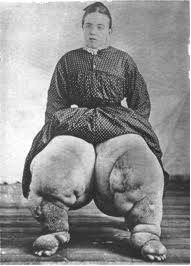
75 years of lipedema as a known condition and we don’t even have that! Dr. Veraart called the number of parameters ‘limited’. In plain English that would be something like: there are only so many (known) symptoms linked to lipedema. · Lipedema often coincides with: venous insufficiency, flat feet, obesity and lymphatic insufficiency.
· Other types of fat depositions do exist. Abnormal fat deposits on the legs is not necessarily lipedema.
Dr. Veraart mentioned in this context Madelung, lipodystrophy and lipoatrophica semicularis. Here’s the catch: he said sometimes abnormal fat deposits on the legs are actually from a different disorder. · The cause of lipedema is unknown.
This is where it got really interesting, because he did mention the latest theories. Dr. Mortimer is looking into the genetic aspects and studies families. A genetic mutation (Pit 1) has been found in a family, but in men. For this reason dr. Veraart didn’t think this was the genetic insight that would explain lipedema. What is known is that our fat cells look irregular, all inflamed and ‘drenched with unrest’. Present theories evolve around an interaction between capillaries, fat and muscles. There’s also a theory where the endothelial cellsplay a central part; where they (want to) look into the growth factor of these cells and the effect of hormones.
He also speculated about a possible neurogenic effect - you’ll have to excuse me for my superficial account, but he went at lightning speed with medical terms and all. Suffice it to say that there are more in-depth theories available. Stuff that doesn’t involve nagging about calories and the effect of lymphedema protocols on lipedema patients, to name but a thing. So, there are theories. Now for the hard part. Dr. Veraart was asked what was keeping ‘them’ from actually researching these theories. Money. That’s what keeping them. Most funds go to oncology and cardio-vascular research. He implied patient initiative would be required to get things moving.
The second lecture was by Ms. Dudek, psychologist, psychotherapist and dietician at the university of Warsaw. You may remember her questionnaire being shared on the forums? It evolved around the quality of life in women with lipedema. For us it doesn’t serve much purpose to rehash that it’s hardly uplifting to deal with an unrecognized and painful condition, rarely diagnosed and mostly fairly late in life and difficult to control, too. However, she did have a few useful insights and points, from the patient’s perspective.
· Lipedema affects all aspects of functioning, including avoiding treatment, thinking nothing would help anyway. Many of us pick up unhealthy eating habits in the broadest sense: overeating, or eating too little, not eating in company, eating disorders.
· Dieting can lead to overeating.
She mentioned in this context the Minnesota experiment, an (old) semi-starvation experiment. · Social isolation she considers to be more harmful than poor diet and lack of exercise.
· Which does help in coping with lipedema is psychological flexibility, which – and this interesting – can be learned to an extent.
As for coping with a new diagnosis she gave these pointers:· Give yourself time, time to experience that mixture of relief and grief.
· Be curious and active.
· Accept what you cannot change, but focus on what you can control.
· Love yourself – behave towards yourself as if you love yourself.
· Build a support network.
· Ask for help.
As for diet: work on long-term dietary changes, consider mindful eating and use a 80:20 ratio in the healthy food choices you make. Paraphrased I would say the idea behind it is to not go overboard, pick something you can stick with and work with realistic goals. This is part 1 – more to follow!